The intrauterine device (abbreviated IUD) has been popular for quite a long time among women of childbearing age who have given birth. And despite the high contraceptive effect, most women doubt the need to install an IUD, arguing their refusal by the occurrence of side effects and complications.
With the correct choice of the IUD, the professionalism of the doctor (introduction procedure), taking into account indications and contraindications, this remedy is indeed the most successful method of contraception, which does not require strict self-discipline, as, for example, when taking hormonal pills.
An intrauterine device is
An intrauterine contraceptive device or intrauterine device is a device made of synthetic material (medical plastic), which is inserted into the uterine cavity, which prevents the development of an unwanted pregnancy in it. Modern IUDs are small in size, from 24 to 35 mm, and contain either non-inflammatory metals (copper, silver or gold) or the hormone levonorgestrel (LNG-IUD).
Historical reference
The development of an intrauterine method of contraception began in 1909, when Dr. Richter proposed using a contraceptive made from two silk threads connected by a bronze thread. The invention was not popular. Since 1920, the gynecologist Grafenburg began experiments, creating structures from silkworm threads, and later constructed a ring of silk threads, which was braided with silver wire. But a serious drawback of the ring was its spontaneous expulsion (loss).
Later, in 1961, Dr. Lippes produced an IUD of a serpentine configuration (double S), and although the device is called a Lippes loop or Lipps, its zigzag shape is more like a spiral, which gives the name to modern intrauterine devices - intrauterine device.
Mechanism of action
The intrauterine device has several mechanisms of action:
- Inhibition of ovulation, suppression of ovarian function
While wearing an IUD, the hypothalamic-pituitary system is slightly activated, which leads to a slight increase in LH secretion, but to the preservation of the production of estrogen and progesterone. At the same time, there is an increase in estrogen content and a shift in their peak in the middle of the cycle by 1 - 2 days.
- Preventing or disrupting implantation
In the second phase, there is a more significant increase in progesterone, but a decrease in the duration of the second phase. Although the endometrium changes cyclically, the synchrony of these transformations is disrupted: the first phase is lengthened, and secretory changes are delayed (incomplete maturation of the uterine mucosa), which prevents the introduction of a fertilized egg into the endometrium. Due to the copper content in the coil, the absorption of estrogen is enhanced, and the LNG-IUD stimulates the early maturation of the endometrium and its rejection, when the egg has not yet had time to securely attach itself in the uterus. This is the abortive effect of the spiral.
- Impaired sperm movement and aseptic inflammation in the uterus
The IUD, while in the uterus, irritates its walls, which provokes the uterus to secrete prostaglandins of biologically active substances). Prostaglandins not only stimulate the release of LH and inadequate maturation of the endometrium, but also aseptic inflammation in the uterus. At the same time, the level of prostaglandins increases in the cervical mucus, which inhibits the penetration of sperm into the uterine cavity. As a result of aseptic inflammation, which arose in the uterine cavity in response to the insertion of the IUD as a foreign body, the content of leukocytes, macrophages and histiocytes increases. All of these cells enhance phagocytosis (devouring) of sperm and isolate the fertilized egg, preventing it from implanting in the endometrium.
- Changes in the nature of movement of a fertilized or unfertilized egg through the fallopian tube
The released prostaglandins accelerate the peristalsis of the fallopian tubes, as a result of which either an unfertilized egg enters the uterus and meets the sperm in the tube, or a fertilized one, but too early, when the endometrium is not yet ready for its implantation.
Types of intrauterine devices
Intrauterine devices can be of various types, and differ both in shape and in the content of medicinal substances or metal in it.
In addition, as new intrauterine devices are developed, all IUDs are divided into 3 generations according to the time of their appearance:
1st generation IUD
Such spirals are made of plastic and do not contain any metal, so they are classified as inert (neutral). The contraceptive effect is achieved only by provoking aseptic inflammation and preventing the implantation of a fertilized egg. The Lippes loop belongs to the first generation. But their use has been prohibited by WHO since 1989 due to the low contraceptive effect, the high likelihood of developing inflammatory diseases of the uterus and appendages, and spontaneous expulsion.
2nd generation Navy
The second generation of spirals includes metal-containing ones. First, IUDs containing copper appeared, which has an anti-anidation effect, that is, it prevents implantation. Copper-containing spirals consist of plastic (the basis of the IUD), the leg of the spiral is wrapped with copper wire. Depending on the amount of copper, these intrauterine devices are divided into low-copper IUDs and high-copper IUDs. Later, spirals began to be made with silver content in the lumen of the leg or with gold, in the form of a wire wrapped around the leg. Silver- and gold-containing IUDs are considered more effective in terms of contraception (the contraceptive effect reaches 99%), prevent the development of inflammatory diseases, and the duration of action increases to 7–10 years.
3rd generation Navy
The latest generation of IUDs includes intrauterine devices that contain a progestin, levonorgestrel. Their other name is LNG-IUD. Popular hormone-containing intrauterine devices are Mirena and the LNG-20 IUD. LNG-IUDs not only have an almost 100% contraceptive effect, but also have a therapeutic effect (therefore they are recommended for women with small uterine fibroids or endometrial hyperplasia).
Spiral shapes
IUDs differ not only in composition, but also in shape. Today there are about 50 types of spirals of different shapes. The form and composition of the intrauterine contraceptive is recommended and selected by the doctor based on medical history, body type, individual anatomical characteristics, and other things. Therefore, it is difficult to decide “on the spot” which intrauterine device is better. Popular spiral shapes:
Semi-oval
Another form of intrauterine contraceptive is called an umbrella or horseshoe. There are small spikes on the external protrusions - the “shoulders” of the spiral, which allow the device to be securely fixed in the uterine cavity and prevent its expulsion.
Among the advantages, one should note their almost painless insertion (the spiral is well configured when passing through the cervical canal, and straightens out in the uterine cavity), rare spontaneous falls of the device due to the spikes on the “shoulders,” and a minimum of painful sensations when worn. “Horseshoes” are ideal for women who have a history of spontaneous childbirth or women whose cervix is “nulliparous” (after surgical birth).
Round or semicircular
Another name for such contraceptives is a ring or half ring. In China, IUD rings that do not have “antennae” and have one curl are popular.
From practice: Ring-shaped spirals are quite inconvenient. Mostly, patients complain of pain, in some cases quite significant, at the time of insertion of the spiral. The “ring” is poorly configured and passes through the cervical canal with difficulty, which causes pain. In addition, women with a history of only one birth often complained of painful menstruation. Therefore, in my opinion, this form of contraception is absolutely not suitable for women after a cesarean section or who have only one independent birth. But multiparous patients did not complain either during insertion or during wearing. The contraceptive effect, despite the shape of the device, remains high.
T-shaped
Perhaps the most common type of spirals in Russia. Externally, the contraceptive resembles the letter “T”, that is, it has a rod wrapped in copper or silver (gold) wire and 2 “shoulders”. If we talk about the best intrauterine devices, then this form is the most preferable, it is so easy to insert, comfortable to wear (the woman does not experience discomfort), removed without problems and securely fixed in the uterus due to the flexibility of the “shoulders”.
In my opinion, the T-shaped spiral has only one drawback - its percentage of spontaneous expulsion is higher than that of spirals of other shapes. Recommended for women after a cesarean section or after a single spontaneous birth (the cervical canal is more or less closed, which reduces the risk of prolapse).
Review of popular IUDs
Mirena
Contains the most active of gestagens - levonorgestrel, which gives the spiral antiestrogenic and antigonadotropic properties, in addition to a high contraceptive effect. Levonorgestrel suppresses the proliferation of the endometrium and causes its atrophic changes, therefore this contraceptive is administered more often for therapeutic purposes (for dysfunctional uterine bleeding, heavy and prolonged periods, dysmenorrhea, uterine fibroids, premenstrual syndrome). Mirena is also used as hormone replacement therapy in post- and perimenopause. Guaranteed service life 5 years. Its shape is T-shaped.
The average price of Mirena spirals is 12,000 rubles.
Juno Spiral
Has many varieties:
- Juno Bio-T in the form of a horseshoe or ring with a copper component;
- Juno Bio-T Ag in the shape of a horseshoe or the letter “T” with a copper-silver component;
- Juno Bio-T Super, made in the shape of a “T” letter, contains copper and propolis, which provides an anti-inflammatory effect;
- Juno Bio-T Au – contains gold, suitable for women with allergies to metals.
Due to its composition, this type of spirals has a general antiseptic effect, that is, the risk of inflammatory diseases of the uterus and appendages is quite low. Therefore, the Juno spiral is recommended for patients with chronic adnexitis or endometritis.
The average price of a Bio-T Ag spiral is 400 rubles.
Nova-T Cu Ag
Guaranteed service life up to 5 years. It is made in the shape of the letter “T”, the leg of the device is wrapped in copper wire with a silver core (silver slows down the corrosion of copper, lengthening the life of the spiral).
An effective contraceptive with a fairly long wearing period. Recommended for young women with 1-2 births and previous inflammatory diseases of the uterus or appendages.
The average price of a Nova-T spiral is 2500 rubles.
Multiload
Made in the shape of a horseshoe with spikes on the outer surface of the hanger. The rod of the device is wrapped with copper wire. There are 2 types of Multiload spirals available (depending on the copper surface area): Cu-250 (copper area 250 square mm) Cu 375 (375 square mm). The validity period is 5 and 5 – 8 years, respectively.
Perhaps the best spiral of all those on the market today. It is easy to insert and wear, the duration of action is long, the contraceptive effect is high, and it has antiseptic properties (due to copper). As a rule, gynecologists recommend Multiload to women who decide to introduce the device for the first time.
The average price in Moscow is 3,500 rubles.
Gravigard – Cu-7
Made in the USA in the shape of the number 7, the leg is covered with copper wire (copper area 200 cubic mm). Installed for 2 – 3 years.
Since the device has only one “shoulder”, it is inserted almost painlessly, therefore it is suitable for nulliparous women, including those whose first birth ended in a cesarean section. The risk of the IUD falling out in this case is very low, but it is recommended to wear Gravigard Cu-7 for women with high parity (three or more births).
Validity period of the IUD
How long can a spiral last? A similar question worries all women who decide to use this contraceptive method. The service life of the IUD varies for different types of intrauterine contraceptives and depends on the amount of metal or drug included in their composition (in the absence of side effects while wearing the device):
Duration of use depends on the total surface area of the copper. The validity period ranges from 2 – 3 years to 5 – 8 years.
Service life from 5 to 7 years.
Validity period is from 5 to 7 years, longer wearing is possible, up to 10 years.
LNG-IUD
Contraceptive and therapeutic effects are guaranteed for 5 years of wearing the contraceptive, but persist for 1 to 2 years after the end of the official validity period.
Insertion of an intrauterine contraceptive device
Before you decide to install an intrauterine device, you should visit a gynecologist and undergo the necessary examination:
- a thorough history taking and gynecological examination to identify contraindications for the use of an intrauterine device;
- taking smears for microflora from the cervical canal, urethra and vagina;
- PCR for sexually transmitted infections (according to indications);
- CBC (exclude anemia, allergic reaction - increase in eosinophils and hidden inflammatory process);
- UAM (rule out urinary tract infection);
- Ultrasound of the pelvis (exclude gynecological diseases, pregnancy, including ectopic, and uterine malformations);
- colposcopy (according to indications: background processes of the cervix).
On the eve of the procedure for introducing a contraceptive, it is recommended:
- maintaining sexual rest for 2 – 3 days before the procedure;
- refusal to douche and use intravaginal products (suppositories, tablets and creams);
- refusal to use intimate hygiene products.
The IUD is inserted at the end of menstruation, approximately on the 4th - 5th day, which prevents its loss (menstrual bleeding decreases, and the external pharynx still remains slightly open, which facilitates the introduction of a contraceptive).
Administration procedure
- the patient is placed on a gynecological chair, a Simps speculum is inserted into the vagina, exposing the cervix, the cervix and vagina are treated with an antiseptic (the procedure is performed on an outpatient basis and is practically painless);
- the cervix is fixed with bullet forceps, the length of the uterus is measured with a probe;
- a plastic conductor (attached to the IUD) is inserted into the cervical canal, which is advanced into the uterine cavity, then the contraceptive is pushed out with a plastic piston (ideally, the spiral should rest against the uterine fundus with its “shoulders”); if the spiral is T-shaped, the “hangers” are first tucked into the conductor (by pulling the threads from the back side of the conductor);
- the conductor is carefully removed, long threads protrude from the cervix into the vagina, which are cut to the required length, creating “antennae” - they will protrude from the external pharynx, which is necessary for self-control of the presence of the IUD in the uterus;
- the entire administration process takes no more than 5 minutes.
After introduction
- the doctor records the date of installation, the model of the device in the outpatient card and informs the patient of its validity period;
- control appearance is scheduled after 10 days;
- sexual rest, refusal to lift heavy objects, take laxatives and hot baths for 14 days after insertion of the intrauterine device;
- refusal to use vaginal tampons (7 – 10 days).
Immediately after the procedure, the woman is recommended to sit, and if necessary, lie down, for 15 to 30 minutes. Pain in the lower abdomen may occur (contractions of the uterus in response to the presence of a foreign body in its cavity), which should disappear on their own after 30 - 60 minutes.
A woman should be checked regularly (once every six months) by a gynecologist and independently monitor the location of the contraceptive (feeling the “antennae” with her fingers at the external pharynx). If the “antennae” cannot be felt or the lower end of the device is felt (incomplete spontaneous expulsion), you should urgently contact a specialist. Other reasons to see a doctor are:
- delayed menstruation (possible pregnancy);
- bleeding or intermenstrual discharge with blood;
- pain in the lower abdomen (intense during menstruation and discomfort outside of menstruation);
- fever, signs of intoxication;
- the appearance of pathological vaginal discharge (with an odor, greenish or yellowish in color, foamy, abundant);
- pain during coitus;
- increased menstrual blood loss (lengthened periods, increased volume of blood lost).
Contraindications and complications
The introduction of an intrauterine contraceptive has a number of contraindications.
The absolute ones include:
- pregnancy or suspicion of it;
- genital cancer, suspicion of it or hereditary predisposition;
- acute and exacerbation of chronic inflammatory diseases of the genitals;
- promiscuous sex life (high probability of contracting sexually transmitted infections);
- bleeding from the genital tract of unknown etiology;
Relative ones include:
- inflammatory processes in the past of the uterus/appendages;
- chronic inflammatory diseases of the uterus/appendages;
- painful periods;
- heavy, prolonged menstrual or intermenstrual bleeding;
- hyperplastic processes of the endometrium;
- endometriosis;
- underdevelopment of the uterus and malformations (septum in the uterus, bicornuate or saddle-shaped uterus);
- ectopic pregnancy in the past;
- cervical deformity, anatomical isthmic-cervical insufficiency;
- anemia and other blood diseases;
- absence of childbirth;
- taking immunosuppressants;
- chronic inflammatory general diseases, including tuberculosis;
- cardiovascular diseases;
- cervical canal stenosis;
- submucosal fibroid;
- intolerance to metals or hormones;
- spontaneous expulsion of the IUD in the past.
Side effects and complications
Possible complications and adverse reactions during or after insertion of an intrauterine device include:
- cervical injury, bleeding and perforation of the uterus during the introduction of a contraceptive;
- intense pain during menstruation, during sexual intercourse, during the intermenstrual period;
- spontaneous expulsion of the contraceptive;
- cycle disturbances (extension of menstruation, heavy periods, intermenstrual bleeding);
- pregnancy, including ectopic;
- chronic endometritis and adnexitis after removal of the IUD, infertility;
- anemia (with hyperpolymenorrhea);
Advantages and disadvantages
The use of intrauterine contraception has its advantages and disadvantages, like any other method of protection against unwanted pregnancy.
Advantages of the Navy
- acceptable price;
- duration of use;
- financial savings (no need to constantly buy birth control pills and condoms);
- does not require strict self-discipline (constant taking of pills);
- rapid restoration of reproductive function after removal;
- high efficiency (up to 98 – 99%);
- the occurrence of a contraceptive effect immediately after administration;
- the possibility of emergency contraception after unprotected coitus;
- therapeutic effect (for fibroids, heavy periods, intrauterine adhesions - synechiae);
- relaxation during intimacy (lack of fear of getting pregnant);
- suitable for contraception in the postpartum period;
- absence of adverse reactions and complications when taking into account contraindications and correct selection and administration of a contraceptive;
- compatibility with medications and alcohol;
- anti-inflammatory effect due to the content of copper, silver, gold and propolis.
Disadvantages of the IUD
- increased risk of ectopic pregnancy (except LNG-IUS);
- the risk of spontaneous (and unnoticed by the woman) loss of the contraceptive;
- increased risk of contracting sexually transmitted infections and the occurrence of adnexitis/endometritis during casual sexual intercourse;
- an increase in the volume and duration of menstrual blood loss and the development of anemia;
- risk of damage to the uterus or cervix when inserting or removing a contraceptive;
- requires regular checking for the presence of a spiral;
- the onset of intrauterine pregnancy and, as a rule, the need to terminate it;
- the main effect of the IUD is abortifacient, which is not acceptable for religious women;
- the introduction and selection of the spiral is carried out by a specialist.
Insertion of the IUD after...
Optimal timing for insertion of an intrauterine contraceptive device:
- 6 weeks after spontaneous childbirth (healing of the wound site in the uterus after separation of the placenta and formation of the cervical canal);
- six months after surgical birth (final healing of the uterine scar and its consistency);
- after 35 years in the absence of contraindications or in the presence of endometrial hyperplastic processes (LNG-IUS);
- after an abortion, either immediately or during the first menstruation;
- after unprotected coitus for 5 - 7 days.
Question answer
Question:
I want to try installing an IUD. What is the best spiral?
No gynecologist will give an unambiguous answer to such a question. The doctor observing you can only recommend one or another form of device with a certain composition. The choice depends on previous inflammatory diseases of the pelvic organs, hormonal disorders (whether there were dysfunctional bleeding, disruptions in the cycle or hyperplastic processes), the number of births and their resolution (independent or surgical), constitutional characteristics (physique, uterine curvature) and other factors. And even after a thorough study of the medical history and examination, it is impossible to say with confidence that this particular spiral will be suitable. When choosing a device, you should focus not on the price (the more expensive, the better) and not on the advice of friends (I have this shape and brand, no problems), but on the doctor’s recommendations. Choosing and installing an IUD is comparable only to choosing shoes. Until you try it on, you won’t know whether the shoes fit or not, it doesn’t matter that the size matches (the shape of the last, the width of the foot, the instep, and much more are important). The same can be said about spirals. Even after successful insertion and safe wearing for a month, such severe pain may occur during menstruation that the patient runs to the doctor with a request to remove the device.
Question:
When I independently checked the presence of a spiral, I did not feel the “antennae”. What to do?
You need to see a gynecologist. It is possible that the IUD fell out without you noticing, so pregnancy is possible. But it is possible that the “antennae” simply “hid” in the cervical canal, and the gynecologist will remove them with tweezers and gently pull them.
Question:
Is it possible to get pregnant while using the IUD?
Yes, this method does not have a 100% contraceptive effect. Pregnancy is possible in 1–2% of women. Its risk is especially high with incomplete spontaneous expulsion, when not only “antennae” protrude from the external pharynx, but also the rod of the spiral.
Question:
When and how is the spiral removed?
If wearing a contraceptive does not cause discomfort and does not cause side effects, then it is removed either after the expiration date or at the request of the woman, on any day of the cycle (preferably during menstruation - less painful). Removal is performed by a gynecologist by grasping the “antennae” with tweezers or a forceps and pulling them towards himself. A situation is possible when the spiral threads are not visible in the outer pharynx or come off when grasped with a forceps. Then the IUD is removed with a special hook, inserted into the uterine cavity and hooking the contraceptive onto the “shoulders”. Sometimes the situation requires short-term hospitalization to remove the device with a hook and subsequent curettage of the uterine cavity (significantly exceeding the period of wearing the IUD, failure of an attempt to remove the device on an outpatient basis, uterine bleeding or excessive growth of the endometrium, confirmed by ultrasound).
Question:
How quickly is the ability to become pregnant restored after the device is removed?
The timing of fertility restoration varies from person to person. But the occurrence of a desired pregnancy is observed in 96% of women throughout the year.
Question:
How long does it take for a spiral to take root?
If the IUD is selected correctly, taking into account the size and length of the uterus, contraindications and anatomical features, then it “takes root” in about 1 – 3 months.
Question:
The husband complains of the feeling of the spiral threads during sexual intercourse. Is this normal and what should I do?
If your husband does not like these sensations, perhaps you were left with too long “antennae” after the introduction of the contraceptive. You can contact your gynecologist with a request to shorten them somewhat (but there is a high probability of their subsequent disappearance in the cervical canal, which will complicate self-monitoring for the presence of a spiral).
Question:
When can a new coil be installed after removing the old one?
If the IUD did not cause adverse reactions, a new one can be installed in a month, but better after 3, to make sure that the menstrual cycle is normal and undergo additional examination.
One of the most effective methods of female contraception is the intrauterine device. The reliability of this method of contraception is about 98%, which is a very high result.
Let's take a closer look at what the action of intrauterine devices is based on, what reviews women have about them, what examinations need to be done before installation, who can get the device and who cannot, what are the indications and contraindications, as well as possible complications.
The action and effectiveness of the intrauterine device
An intrauterine device is a small plastic device (most often), which, when inserted into the uterus, blocks the possibility of a fertilized egg entering the uterine cavity and further development of the embryo. Some women consider the IUD to be an abortifacient method of contraception, since fertilization still occurs. For some religious people this is unacceptable. For such people, from a moral point of view, the Mirena intrauterine device is more suitable.
It not only mechanically prevents pregnancy, but also prevents fertilization from occurring due to changes in hormonal levels (this device releases a small amount of the hormone levonorgestrel daily - 20 mcg per 24 hours, this action is similar to the action of oral contraceptives). Reviews about the Mirena intrauterine device are positive; there are no “punctures” due to its dual action. Read more about women's opinions and discussions in the comments at the bottom of this page.
It is recommended to install intrauterine contraceptives for women who have one healthy partner, since they do not protect against sexually transmitted infections. And in case of infection, they can become a catalyst for the inflammatory process in the uterus.

Types of intrauterine devices
There are several types of intrauterine systems. They differ from each other in the material from which they are made, in size and shape. Only a doctor can choose the right intrauterine device. The most popular intrauterine devices: Nova T, Multiload, Juno, Mirena.
But talking about which of these intrauterine devices is the best is wrong. Each of them has its pros and cons. In addition, the IUD must be selected individually for each woman. You can buy an intrauterine device at almost any pharmacy. But before purchasing, we would recommend calling several pharmacies at once to find out their price, as it can vary greatly.
The Nova T spiral (price about 2500 rubles) has a T-shape. Its horizontal branches are very elastic, which makes the installation of the IUD easier and non-traumatic. This device can remain in the uterus for up to 5 years.

The Multiload intrauterine device (price - about 3,500 rubles) has the shape of a semi-oval, at the ends of its branches there are spike-like protrusions that allow the device to better attach to the walls of the uterus. This feature reduces the risk of spontaneous prolapse (expulsion) of the IUD.

The Mirena IUD is considered one of the most effective, but also expensive IUDs. The cost of this intrauterine device is about 7,000-10,000 rubles. The validity period of Mirena is 5 years. Installation of the Mirena coil for small fibroids is also acceptable, and some experts even believe that this “hormonal coil” can slow down the growth of this benign tumor.
The big advantage of expensive IUDs is that the materials they contain (gold, silver, copper) have an anti-inflammatory effect.

Juno Bio
Juno spirals appeared in Russia more than 20 years ago. They were invented by Belarusian doctors. Copper-containing IUDs have become a real breakthrough in the field of contraception. Now in pharmacies you can find several varieties of this contraceptive - both for women who have given birth and for women who have not given birth.

The most budget option. Its cost is about 250 rubles. This is a T-shaped spiral, shaped like an anchor. It is made of inert material and covered with very thin copper wire. Copper has an additional contraceptive effect. Shelf life - 5 years.
Juno Bio-T Super
Approximate cost - 300 rubles. Its difference from the previous model is the special antimicrobial composition with which the spiral is treated. This composition includes propolis. According to the manufacturer, this serves as a prevention of endometritis and ovarian inflammation - common complications when using an IUD. The period of use is 5 years.
Juno Bio-T Ag with silver
Price - about 450 rubles. Silver is part of the “winding” of the spiral leg, along with copper. This precious metal prevents the oxidation of copper and thus improves its efficiency. Can remain in the uterus for up to 7 years.

The price is about 550 rubles, with copper. It is distinguished by its f-shaped shape, jagged edges and slightly larger size than previously described IUDs. Therefore, this IUD should be used by mothers with many children, women who have had several abortions, as well as those who have already had cases of an intrauterine contraceptive falling out of the uterus. Service life - 5 years.
Costs approximately 800 rubles. The composition includes not only copper, but also silver. Shown to the same women as Juno Bio Multi. But the service life is longer - 7 years.

Ring-shaped Juno Bio-T
Approximate cost - 300 rubles. This is the only IUD that can be recommended for installation in nulliparous women. It has a relatively small size (18 mm) and a shape that minimizes the risk of perforation of the uterine wall by the spiral. The second type of spiral has a slightly larger size - 24 mm. It is recommended for women who have given birth, but for those who for some reason cannot use a classic T-shaped IUD. If after its installation there was severe bleeding, pain, etc. It can remain in the uterus for up to 5 years. Contains copper.
Ring-shaped Juno Bio-T AG
Costs about 450 rubles. The properties are the same, but contains silver. Established for a period of up to 7 years.
This is an expensive spiral with gold, it costs about 5,000 rubles. Has a T-shape. This coil is used by those who have an allergic reaction to copper. It can lead to contraceptive rejection and loss. The spiral with gold has much less side effects, since it has an anti-inflammatory effect, even greater than silver. Validity period - 7 years. The appearance is exactly like the regular Juno Bio-T.
By the way, there are more expensive IUDs on our market, for example T de Oro 375 Gold - a spiral with a gold core, its cost is more than 10,000 rubles. Manufacturer - Spain.

Installation of an intrauterine device
Before installing an intrauterine device, you need to undergo a gynecological examination and take smears. The spiral is installed only in healthy women who have given birth more often and who do not have inflammatory processes in the reproductive system at the time of IUD installation. It is also recommended to do an ultrasound to detect possible contraindications to this type of contraception.
The installation of an intrauterine device is carried out 5-7 days from the beginning of the menstrual cycle, when the cervical canal is slightly open, this will make the whole process easier. A contraceptive can also be installed immediately after an abortion, 5-6 weeks after childbirth (if by that time the uterus has contracted, and even if the menstrual cycle has not yet returned) and within 3-4 days after unprotected intercourse for the purpose of post-coital contraception.
Before installing the IUD, the gynecologist performs a gynecological examination and measures the length of the uterus using special instruments. The installation itself lasts no more than 5-7 minutes, or even less. At this time, a woman may experience unpleasant pulling sensations in the lower abdomen.
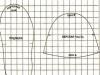
Schematically, the installation of an intrauterine contraceptive looks like this.

Immediately after installation and for 7-10 days, mild pain may persist. The same as spotting and spotting. If they do not cause you much discomfort, then this is within normal limits. It is possible, if necessary, to take painkillers (ibuprofen, paracetamol, etc.) or antispasmodics (No-spa).
After 8-10 days, you can resume sexual activity without fear of pregnancy. But before this time it is better to take care. You should also avoid strenuous physical activity, which includes not only heavy lifting, but also long walking. Postpone sports and visiting a bathhouse or sauna for a couple of weeks.
10 days after installation of the intrauterine contraceptive, you should visit a doctor and it is advisable to undergo a control ultrasound if it was not done immediately on the day of the procedure. Visits to the gynecologist also need to be scheduled after 1, 3, 6 months, and then go for examinations 2 times a year.
What women who have an IUD should always remember
1. It is necessary to periodically independently check for the presence of spiral threads protruding from the cervix. Their length should remain the same. If you cannot feel the threads, they have become too long, or vice versa - short, then you need to urgently see a doctor, this means that the IUD has moved out of its place. And if there are no threads, then it is quite possible that expulsion has occurred - spontaneous prolapse of the IUD or the spiral is lost somewhere in the uterine cavity.
2. Even if everything is fine, you need to go to the gynecologist once every six months.
3. In no case should you wear the IUD for longer than the recommended period, since the IUD can “grow” into the uterine cavity and can only be removed from there surgically. Doctors usually recommend removing the intrauterine device several months before its expiration date to avoid complications.
4. Unfortunately, even the IUD does not guarantee 100% non-pregnancy. On average, out of 100 women with an IUD installed, 1 becomes pregnant. Therefore, you need to monitor your menstrual cycle as carefully as before installing the IUD.
5. If you have severe abdominal pain, an unpleasant odor from the genitals, sudden weakness or bleeding, immediately go to the doctor or call an ambulance.
6. If you are planning a pregnancy, then removal of the IUD is mandatory. It (removal), as well as the introduction of an intrauterine device, is performed only by a gynecologist.
Indications and contraindications for IUDs, advantages and disadvantages, pros and cons
1. The IUD is indicated for women who have given birth as a reliable means of contraception.
2. The reliability of the IUD does not exceed 98%.
3. There is a risk (albeit low) of perforation of the uterine wall both during installation and after, the IUD falling out (expulsion).
4. More abundant menstruation, intermenstrual bleeding is possible and, as a result, anemia. When using Mirena this is practically impossible.
5. An IUD cannot be installed in women who have inflammatory or infectious diseases of the external and internal genital organs, neoplasms in the uterus that deform its cavity, or anemia (hemoglobin below 90 g/l). A history of ectopic pregnancy is also a relative contraindication, since its risk always increases in women using this type of contraception.
6. Despite all these disadvantages, intrauterine devices also have undoubted advantages - they are one of the most reliable methods of modern contraception (along with condoms and oral contraceptives), and have a long validity period (up to 7 years).
Pregnancy and intrauterine contraceptive
If pregnancy does occur while using an intrauterine contraceptive, then the woman has two options - either try to save the child or have an abortion. In most cases, you can try to save the child. There are many women who have carried and given birth to healthy children conceived using this type of contraception.
If a woman chooses an abortion, the method of carrying it out will depend only on the duration of her pregnancy, her desire and financial capabilities. First, the doctor removes the device from the uterus, pulls it out by the antennae, then expands the cervical canal and removes its contents either using a curette or a vacuum aspirator.
If the pregnancy needs to be continued, the doctor weighs the pros and cons and decides what would be safer - to immediately remove the IUD or leave it until birth. The specific location where the egg was implanted is of great importance. Removing the IUD can cause spontaneous miscarriage. And a foreign body in the uterus can always become a source of inflammation.
If it is decided to leave the IUD, then it will be “born” along with the afterbirth (placenta) or will be removed from the uterus during a cesarean section.
Discussion: 416 comments
What does your doctor say about pregnancy? Cervical treatment varies greatly... Which one did you undergo? What's wrong with your cervix now? Are there any problems?
The risks after “cauterization” and conization are that the cervix, due to the scars formed as a result of treatment, may either open poorly during childbirth, or, worse, begin to open much earlier than the PDR, that is, there is a risk of late miscarriage or premature birth .
The doctor must determine these risks and the period for postponing pregnancy for you individually.
Hello! A year ago I was treated for erosion, now I’m pregnant. What are the risks if I leave the child, since after erosion I can’t get pregnant for 2 years?
Girls, remember: ANY contraceptives cause irreparable harm to your body. And not only yours.
I will share with you my bitter personal experience, and if this helps at least one of you “decide on the choice of contraception,” then my review was not in vain. My first pregnancy was unplanned, I gave birth to a child at a fairly young age. My gynecologist advised me to immediately put in an IUD shortly after giving birth, because... “The low position of your uterus is conducive to pregnancy.” I considered the spiral to be an ideal contraceptive option, because... I didn’t have to take crap pills, etc. My IUD was also convenient to use; I didn’t have any problems with it, except for heavy periods. I was happy! Especially from the fact that I’m not killing anyone + that I’ll get pregnant when I want!.. After the first IUD, I didn’t hesitate to get a second one. As a result, I had two spirals, 5 years each. Now about health. This is my second marriage and, of course, my husband and I wanted to have a child/children together. We have been married for 9 years, but we still don’t have children together. During these 9 years I had an ectopic twice and that’s all. Both were examined; no pathologies were found in either; anatomically, everything was normal in both. A couple of years ago, my husband, during his free time at work, began translating a book about abortion, “The Right to Life,” into German; we live in Germany. One day I got a call from him: “You said you installed a spiral for yourself? How long did you have it? Five years??? This is a lot!.. I’ll bring the book and you can read it...” I lied to him then. I couldn’t admit that I had two for 5 years each... It turns out that they simply HIDE a lot from us - especially information about the consequences, about how conceived embryos die... The worst thing is ignorance. From ignorance of exactly how many souls I ruined with my IUDs.. Having re-read the truthful literature about the intrauterine device, I realized my terrible mistake.. I am writing to you because not a single “medical” institution will tell you such consequences of the intrauterine device as pathology of ectopic pregnancy and infertility. Regarding infertility from IUDs: there are now a lot of infertile couples among young people and there is already an opinion among people that French IUDs for export are impregnated with some substance that leads to infertility..
In conclusion, I would like to remind women who have an unplanned pregnancy my favorite saying: “God gave a child, he will give for a child!” And this is not even a saying, but a physical law of life that works 100%, believe me!..
They offered me a choice of 2 spirals, Nova for 4700 rubles and Juno for 1500 rubles. The gynecologist says that there is no difference, so why is the price 3 times higher? Maybe someone knows?
Hello. I also want to install a spiral. The doctor recommended copper. Hormonal pills are not very good. I feel bad when taking them. I don’t want to have sexual intercourse and I’m depressed.
Natalya, have you ever tried taking birth control pills? Those for regular contraception? If so, how were you doing with your weight then?
And I don’t understand, Mirena is prescribed for contraception or for what?
Girls, my gynecologist advised me to put Mirena on, but I’ve read so much about the side effects - it’s terrible, and weight gain, and baldness, and wild mood swings (like depression) ... I just cured my hair, in 2010 I lost 35 kg, I’m holding on I’m still at this weight, I got married and don’t want to get hysterical with my husband, my character is not angelic anyway, but I don’t need protection. So what should I do? How to make the right decision?
Eva, yes, no one can select a spiral better than a gynecologist.
I noticed the Juno Bio-T AG spiral. Please tell me if it is suitable for me if I did not give birth, but had one abortion at the 11th week of pregnancy? And what about the size of the spiral: in this case, is it better to use 18/24 mm or is it individual and should you consult a gynecologist?
You know, I am a mother of four children, all my hope was in the IUD, but alas, I was pregnant for 6 months and did not dare to give birth. The children are small, well, as much as possible, it’s hard, of course, I’m sorry. What now, what to do...
There are several types of Juno (see article for information). The shelf life of spirals is 5-7 years, this is the maximum period for how long they can be kept without changing. But the doctor can remove the IUD at your first request.
According to statistics, out of 100 women using an IUD, 3 become pregnant. If you look at the comparison, the number of unplanned pregnancies is higher when using a condom and lower when using a condom.
Nowadays, it is not difficult to find an effective means of contraception. A married couple has the right to choose a method independently, taking into account all the pros and cons. It is very important to visit a doctor and consult on this issue. After all, the health of a woman who wants to become a mother or already has children primarily depends on this. One of the most popular methods is the intrauterine device. Let's look further at the pros and cons of the intrauterine device.
How does the IUD work?
The purpose of the IUD is to protect against unplanned pregnancy. The name suggests that it is inserted into the uterine cavity, and it was obtained due to the previous appearance of the product, as it looked like a spiral. Currently, the IUD is a T-shaped stick made of flexible inert plastic. This material is completely safe for women's health.
There are two types of spirals:
- The upper part of the spiral is in the form of a thin copper wire.
- The spiral contains a container with hormones that enter the uterus throughout its entire lifespan.
It has both the first and second types of pros and cons. The photo above shows what this type of contraception currently looks like.
The principle of operation of the spiral:

Who can install a spiral:
- A woman who has given birth and is over 35 years old.
- Women who have children after an abortion without complications.
- Without cervical pathologies.
- If you protect yourself with oral contraceptives, it is not recommended.
- Women who have a low rate of sexually transmitted infections.
Contraindications to the IUD
Before using this method of contraception, it is necessary to consider all the pros and cons of the intrauterine device.

And also make sure that there are no following contraindications:
- There was no birth yet.
- Constant change of sexual partner.
- Cancers of the pelvic organs.
- The presence of injuries and stitches on the cervix.
- Ectopic pregnancy.
- Blood diseases. Anemia.
- Infertility.
- Vaginal infections.
- The presence of inflammatory processes in the reproductive system.
How to prepare for installing a spiral
First of all, you need to select a suitable spiral and undergo an examination, which includes:

Next, the doctor must probe the uterine cavity and determine the distance between the uterine angles. And only after a thorough examination and the absence of contraindications is an intrauterine device installed. The pros and cons of BMC should already be considered by you.
Features of the first days with a spiral
It is worth noting that only a doctor can install and remove an intrauterine device. The following side effects may appear within a few days after installation of the IUD:
- Lower abdominal pain.
- Bloody discharge.

You should also avoid increased physical activity. It is necessary to adhere to proper nutrition, rest more, and lie down.
The manifestation of side effects can be observed for six months and will disappear completely over time.
It is necessary to undergo regular medical examinations after having an IUD inserted. After installation, a month later, then after 3 months, then once every six months.
What are the advantages of the IUD?
If you have chosen a contraceptive method such as an intrauterine device, you need to know all the pros and cons.
Let's look at the positive aspects:
- It does not require special care. After installation, after a period of rehabilitation, it is practically not felt.
- Efficiency is 95-98%.
- Can be installed for several years.
- For many women, the menstrual cycle becomes shorter, and the periods themselves become almost painless.
- It has a positive therapeutic effect for uterine fibroids and other gynecological pathologies.
- Can be used during breastfeeding.
- Does not affect reproductive function in the body.
- The effectiveness remains regardless of taking any medications.
- Economical and convenient. There is no need to follow a dosage schedule or spend money on regularly purchasing contraceptives.
What are the disadvantages of the IUD?

There are also negative aspects of using an IUD:
- There is a high risk of ectopic pregnancy.
- There is no protection against sexually transmitted diseases.
- The risk of inflammatory diseases increases.
- Cannot be used by nulliparous women.
- Painful periods for the first six months.
- Large blood losses are possible.
We looked at the pros and cons of a contraceptive such as an intrauterine device. We will consider the consequences of BMC further.
What complications can there be when using an IUD?
The qualifications and experience of the doctor are of great importance, since correct installation or removal by an inexperienced specialist can lead to removal of the uterus. Knowing the pros and cons of the intrauterine device, you need to know what complications are possible when using it.
Possible complications when using an IUD:
- Perforation of the uterine walls.
- Cervical rupture.
- Bleeding after installation.
- The IUD can grow into the uterus.
- The antennae can irritate the walls of the cervix.
- The spiral may move or fall out if incorrectly selected and installed.
- Pain in the lower abdomen.
You need to urgently visit a specialist if:
- Severe pain appeared in the lower abdomen.
- There is a suspicion of pregnancy.
- Bleeding continues for a long period of time.
- There are signs of infection: increased body temperature, unusual vaginal discharge.
- Pain or bleeding occurs during sexual intercourse.
- The IUD strings have become longer or shorter.
We looked at what an intrauterine device is, the pros and cons of this method of contraception, as well as possible complications. Next, consider patient reviews.

.jpg) Of all the methods of contraception, the IUD is the most reliable and popular. The application of this technique includes strict adherence to operating rules, one of which is the shelf life of the spiral, the presence of contraindications or restrictions.
Of all the methods of contraception, the IUD is the most reliable and popular. The application of this technique includes strict adherence to operating rules, one of which is the shelf life of the spiral, the presence of contraindications or restrictions.
As for how long the spiral is placed, it depends on the manufacturer of the product and the materials used in its manufacture. The hormonal IUD lasts 6 years (plus or minus a couple of years depending on the manufacturer), the copper-containing version is less regulated - the IUD lasts 10 years without the need for replacement. Considering that the contraceptive is actually a foreign body, a woman should carefully monitor how long the IUD is placed and not exceed it, as this can lead to serious side effects.
IUD installation
The IUD is inserted by the gynecologist approximately 3-4 days after the start of menstruation, since it is at this time that the cervix is slightly open, which makes the procedure easier. In some cases, the best time will be 5-9 days after the end of your period. The doctor will determine the best option.
During the first days after installation, minor bleeding is possible. After 1-1.5 months, you need to visit the gynecologist again for examination. You should immediately contact a specialist in the following cases:
- unusual pain, particularly after sexual intercourse;
- severe bleeding;
- spasmodic pain in the lower abdomen;
- absence of menstruation;
- inability to detect contraceptive threads;
- palpation of the hard part of the contraceptive;
- product loss;
- if you use a spiral whose validity period has already expired;
- other atypical symptoms.
When can I remove the intrauterine device?
Regardless of the type and age of the device, it must be removed under sterile conditions by a gynecologist after a preliminary examination. You should not do this on your own, as there is a risk of damaging the uterine mucosa and introducing infection into the body.
If there were no complications or infections during the use of the IUD, then the removal process will be quick and completely painless. If it is impossible to find the threads of the product or other complications arise, hysteroscopy is performed to obtain a more complete picture of the location of the intrauterine contraceptive. The removal process consists of two main stages:
- Inspection and assessment of the condition in which the intrauterine device is located, the period of use of the product at the moment, etc.
- Delete. The optimal time to remove an IUD is during menstruation. This is done using local anesthesia. If we are talking about hysteroscopy, then anesthesia is used. In some cases, in particular, if the service life of the intrauterine device is significantly exceeded, it is impossible to remove the product through the cervical canal, so the contraceptive is removed through the abdominal cavity.
As for when you can remove the intrauterine device, this can be done before the expiration date:
- at the personal request of the woman;
- with partial rejection of the drug by the body;
- when the IUD is displaced, which can be determined by the device’s antennae, which have become either longer or shorter;
- in the presence of acute inflammatory processes in the pelvic organs;
- very heavy bleeding;
- cancer;
- the onset of menopause;
- pregnancy;
- other pathologies.
If the IUD remains in place for longer, there is a possibility that the device has become tightly attached to the walls of the uterus or even grown in. That is why women who use this type of contraceptive should undergo regular examination by a gynecologist, which helps to detect the problem in the early stages. There are cases with patients whose IUD lasts for 20 years or even more. Removal of the product under such circumstances is quite difficult and is usually carried out in a hospital setting.
Removal of the IUD is a common procedure that can be performed regardless of how old the IUD has been in place. In the absence of infection and complications, the process is easy and painless. If there are difficulties with removal, the contraceptive is examined and removed in a hospital setting. The cause of complications can be both the characteristics of the body and failure to comply with operating conditions. In order to protect yourself, you need to regularly visit a gynecologist and take into account how much a particular type of IUD is placed.
Hope asks:
My mother has had an IUD for 26 years, it doesn’t bother her, she doesn’t have periods anymore (she’s 54). The doctor said that if it doesn’t bother her, then go with her! There are no illnesses, what should she do, remove it or what the doctor said ?and what can happen if it is not removed?
Answers Serpeninova Irina Viktorovna:
Your question reminded me of an incident from my practice.
I would like to tell you this case so that you can decide for yourself what to do with the IUD.
Once a few years ago, at an ultrasound appointment, my colleague brought me a postmenopausal granny (menstruation ended about 20 years ago) with pain in the lower abdomen and fever. During an ultrasound, I discovered an IUD (the so-called Lipps Loop, which we have not used for many years) and ultrasound signs of metroendometritis, fluid in the uterine cavity.
Well, in this situation it is necessary to remove the IUD and anti-inflammatory treatment. And then a colleague suggested that I look at the patient in the chair. What did I see in the mirrors: the external pharynx is closed, i.e. against the background of menopause and, probably, an inflammatory process, a natural process of sticking together of the cervical canal occurred. In this case, it is impossible to remove the IUD, and it is inappropriate to treat the inflammatory process without removing the irritating factor. The patient was sent to the hospital, where she underwent surgical treatment.
This is a rare case when activation of the inflammatory process for unknown reasons occurred in postmenopause, but after it I do not see IUDs for anyone in postmenopause, I insist on removal.
Anette asks:
I gave birth in early January (caesarean). After 2.5 months, I was diagnosed with staphylococcus, treated with tarva and, after a control test, a spiral was placed. A week later I noticed a discharge, an ultrasound scan showed that there was something wrong with the internal scar and a smear showed elevated leukocytes, which I don’t know for sure, but there can’t be anything other than thrush or the same staphylococcus (my husband has been gone for 4 months =(((. If necessary to treat (I'm breastfeeding) any of this --- the spiral must be removed. And can I present any claims to the doctor......
Answers Karapetyan Eliz Martinovna:
Good afternoon, Anette! If you do not currently have regular sexual relations, then, to put it mildly, you do not need the IUD, especially if it is placed only for the purpose of contraception. In addition, you have a violation of the normal composition of the microflora, and this, together with the presence of a foreign body in the uterine cavity (spiral), makes the mucous membrane doubly unprotected and can serve as an open gate for the addition of more serious infections. Therefore, you should remove the spiral, undergo treatment, restore the flora, and only then, if the need arises, install the spiral again. Be healthy!
Elena asks:
Is it better to use oral contraceptives or use condoms or other means of protection? Which spiral to choose?
Answers:
Hello, Elena! The intrauterine device and the condom are too different methods of contraception to compare them. If you have a disordered sex life (that is, you have more than one sexual partner), you should not even think about an intrauterine device. Only condoms will protect you from sexually transmitted infections, the risk of contracting which in this case is very high. If you are nulliparous, again an intrauterine device is not indicated, it is better to use condoms or oral contraceptives (for more details, see the article Methods of modern contraception (protection against unwanted pregnancy) on our portal). If you have given birth and do not have significant gynecological diseases that could be a contraindication for the installation of an intrauterine device, you need to consult a doctor who will select the optimal type of device for you, as well as its size. In any case, before you start using one or another method of contraception (intrauterine device, oral contraceptive pill), it is better to consult a gynecologist. Take care of your health!
Olga asks:
Answers Medical consultant of the website portal:
Hello! Removing the intrauterine device is a manipulation associated with the risk of trauma to the mucous membrane of the genital organs. The consequence of a violation of the integrity of the epithelial cover of the uterus and vagina is inflammation and the possible addition of a secondary infection. In such a situation, prophylactic use of anti-inflammatory and antiseptic agents is recommended. It is better to use medicines of natural origin, and not immediately use “heavy artillery”, which can disrupt the natural balance of vaginal microorganisms. Vagikal may be recommended as the drug of choice in this case.
The main active ingredient of the drug is calendula officinalis. Calendula contains salicylic and pentadecylic acids, which cause the death of streptococci and staphylococci and have anti-inflammatory effects. Calendula helps accelerate tissue regeneration and the formation of new functional cells, promotes the orderly development of the vaginal epithelium and also prevents the formation of scar tissue.
Before using the drug, you should consult your doctor. Be healthy!
Christina asks:
Good afternoon. Please tell me, is it possible to play sports with a spiral, hula hoop, pump up the abs, run and just do fitness training. Are there any undesirable types of training, and which ones exactly?
I read in the instructions for the Multiload coil that side effects include pain in the back and pain in the legs. Well, with the back it’s still clear, but what does this have to do with the legs? I’m very interested in this, since I have varicose veins. In advance thanks for the answer!
Answers Wild Nadezhda Ivanovna:
Christina, if you have varicose veins, then excessive physical activity is not really recommended. Swimming is better for you. Hala Hoop is good, but not always great.... The Multiloud intrauterine contraceptive is usually well tolerated and stays in the uterus due to its design. The contraceptive effect is good and expulsion is extremely rare, i.e. shift of the ICH. Those side effects that are in the instructions: “pain in the legs” due to the IUD are possible, but I have not encountered them in my practice. This can be explained by the fact that there may be an individual intolerance to the metal - copper or silver or a combination of copper-silver - an allergic reaction to the metal is possible. Probably the pain occurs due to the occurrence of an aseptic inflammatory process, which can exacerbate a chronic inflammatory process in the uterine appendages, in the pelvis; with the blood flow, reactive inflammation in the venous bed of the lower extremities is possible - but this is a really rare side effect. Sensitive women may experience pain due to irritation of nerve endings. To wear an IUD, there are no contraindications to physical activity; you just need to limit your exercise during menstruation.
Evgenia asks:
They put the coil in a month ago, the blood smears and flows, the doctor said it is taking root, but I also have some kind of blackness that smears and I also have erosion, remove the coil or what do you recommend?
Answers Medical consultant of the website portal:
Hello, Evgenia! It is believed that within three months after the installation of the intrauterine device, the body adapts to it. Which can be manifested by bloody discharge of varying severity. However, if spotting turns into uterine bleeding, this is an indication for removal of the IUD, since such bleeding can cause the development of severe anemia. Heavy bleeding indicates that this method of contraception is not suitable for a particular woman. Discuss further tactics with your doctor. Take care of your health!
Irina asks:
Good afternoon, I have had an intrauterine device for about 25 years. During the abortion, the doctors gave me an IUD without telling me about it. I found out about her 10 years later. I don’t experience any particular discomfort. What are the dangers of using it for such a long time? They say that it can grow into the uterine cavity and can only be removed by completely removing the entire uterus? Thanks for the answer
Answers Medical consultant of the website portal:
Hello Irina! Leaving the intrauterine device in the uterine cavity for such a long time is indeed fraught with complications. The spiral could indeed have become so firmly fused with the mucous membrane of the uterus that it would be very, very difficult to remove it. In such cases, removal of the IUD may result in severe uterine bleeding. If you decide to remove the IUD, contact a gynecological clinic that can perform surgical interventions, so that if complications arise, you can receive the necessary assistance. Take care of your health!
Julia asks:
In November 2009 I installed an IUD, and took tests after installing the IUD, and found out that I had ureoplasmosis, but the doctor did not remove the IUD and prescribed treatment. I took the entire course, but since then my lower abdomen has been hurting and my back has been strained. Tell me, is it possible to become infected with ureoplasmosis while swimming in the sea, since I still don’t know how I could have become infected, I have had one partner for a long time, and is it possible to remove the IUD without waiting for my period? Thank you in advance
Answers Tarasyuk Tatyana Yurievna:
Hello, Julia!
Carry out a control examination for ureoplasma for yourself and your sexual partner. This infection could have come to you a long time ago (of course, not when swimming in the sea) and did not manifest itself in any way, which did not force you to be examined. You must understand that there are several causes of aching pain in the lower abdomen (problems of the spine, urinary tract, gastrointestinal tract). If, with the help of tests, ultrasound and related specialists, the doctor has ruled out such causes, you can remove the IUD. It is best to do this on the 2-3rd day of menstruation, since this way the cervix is less damaged.
INNA asks:
Hello! My question is: if you get pregnant while the IUD is in place, can you give birth? Or abortion?
Answers Medical consultant of the website portal:
Hello, Inna! If pregnancy occurs while using an intrauterine contraceptive, then the device is removed from the uterine cavity at an early stage. This procedure is covered by the prescription of drugs that prevent abortion, and usually takes place without any special complications for the woman and the fetus. A video has been posted on our portal Removing the intrauterine device, which shows the process of removing the intrauterine device. Be healthy!
Albina asks:
HELLO, I'M 36 YEARS OLD, I GAVE BORN 5 MONTHS AGO TO HIS THIRD CHILD. TWO DAYS AGO I INSTALLED A MULTILOAD SPIRAL. THE TEMPERATURE THIS MORNING HAS RISED TO 37.5 DEGREES. IT ACHES IN THE BONES, THERE ARE NO SYMPTOMS OF COLD OR FLU, DISCHARGE: BLOOD WITH MUCU. COULD TEMPERATURE BE THE CAUSE? BE A SPIRAL? THANK YOU IN ADVANCE!!!
Answers Shapoval Olga Sergeevna:
Hello, Albina. If all the rules for inserting an intrauterine contraceptive are followed, there should be no increase in temperature. Perhaps the reason is an insufficiently complete examination before inserting the IUD. It cannot be ruled out that there was an inflammatory process (chronic, sluggish) in the uterine appendages, and the introduction of the IUD contributed to its exacerbation. Before the insertion procedure, the doctor was required to examine you and, optimally, prescribe an ultrasound. If there are signs of an inflammatory process, the insertion of an IUD is contraindicated. Also, you should have taken a smear for flora and, if an inflammatory process in the vagina was diagnosed, treatment should be prescribed and only then an IUD should be inserted. If sexually transmitted infections are suspected, it is recommended to exclude their presence and, if necessary, treat with subsequent laboratory monitoring. When an infectious process is diagnosed, the spiral promotes its spread into the uterine cavity and appendages. In any case, you need to be examined by the doctor who installed the intrauterine contraceptive to exclude the development of complications. Self-medication is not recommended.
Allah asks:
The IUD has been in place for 14.5 years now. My periods are regular and painless. At the medical examination, doctors say the IUD is in place normally. Does it need to be removed?
Answers Petrenko Galina Alexandrovna:
Hello Anna.
Any spiral should not stand for more than 5 years. Conventional non-hormone-containing intrauterine devices are installed for a period of 3 years, levonorgestrel-containing Mirena devices are installed for a period of 5 years. A longer stay of the IUD in the uterine cavity can contribute to the oxidation of the metal contained in the IUD core, the development of chronic inflammatory processes in the uterus, and contribute to the development of a background for precancerous conditions. I recommend that you remove the spiral with a mandatory cytological examination of the print from the spiral.